Measles update
October 7, 2025
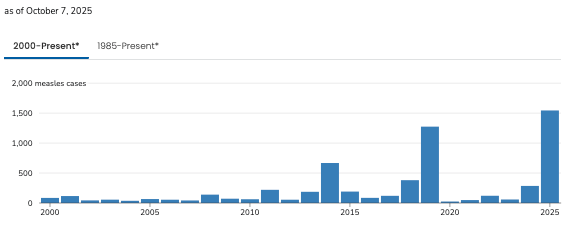
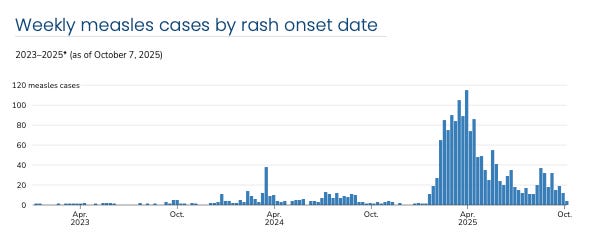
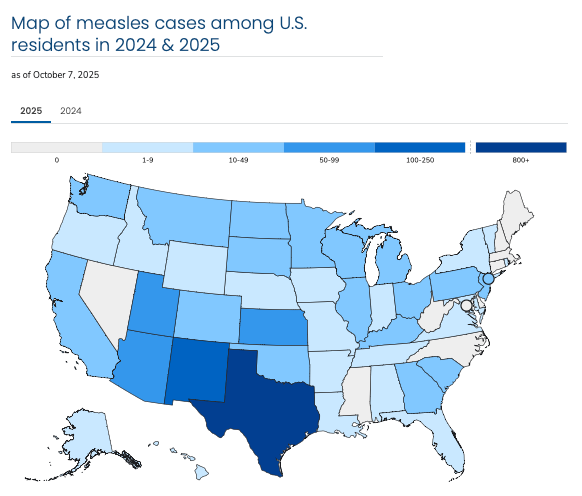
As of October 7, 2025, a total of 1,563 confirmed measles cases were reported in the U.S. for the 2025 season, with 193 hospitalizations (12% of cases) and 3 measles-related deaths in outbreaks still ongoing since January. 1,542 measles cases have been reported by 42 jurisdictions: Alabama, Alaska, Arizona, Arkansas, California, Colorado, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Missouri, Montana, Nebraska, New Jersey, New Mexico, New York City, New York State, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, Virginia, Washington, Wisconsin, and Wyoming, and 21 measles cases were reported among international visitors acquired while visiting in the U.S. A total of 44 outbreaks since January 2025 have been identified, with the ongoing outbreak in West Texas contributing 762 - nearly half - of these cases.
(updated figures, published weekly on Wednesdays by the CDC, can be found here).
This is the largest outbreak of measles since endemic transmission of measles was declared “eliminated” (from domestic endemic transmission) in the U.S. in 2000.
Local transmission has been ongoing since January,
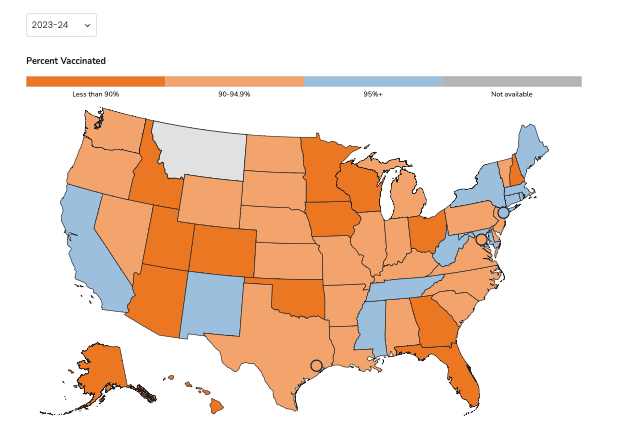
threatening the declaration of “measles elimination” (elimination of domestic endemic transmission) made in 2000. The official definition of domestic endemic transmission involves ongoing transmission over a 12 month period, so “elimination” status would be lost if these outbreaks continue into January 2026, which at this point appears likely, as outbreaks with local community transmission extend to Minnesota, Wisconsin, South Carolina, North Dakota, Arizona, Utah, NYC, and other localities in which MMR vaccination coverage is low. Canada is due to formally lose its measles “elimination” status, declared in 1998, on October 27 2025. Mexico was declared free of endemic measles in 1996, and is due to lose that status if outbreaks continue into February 2026, which currently appears likely.
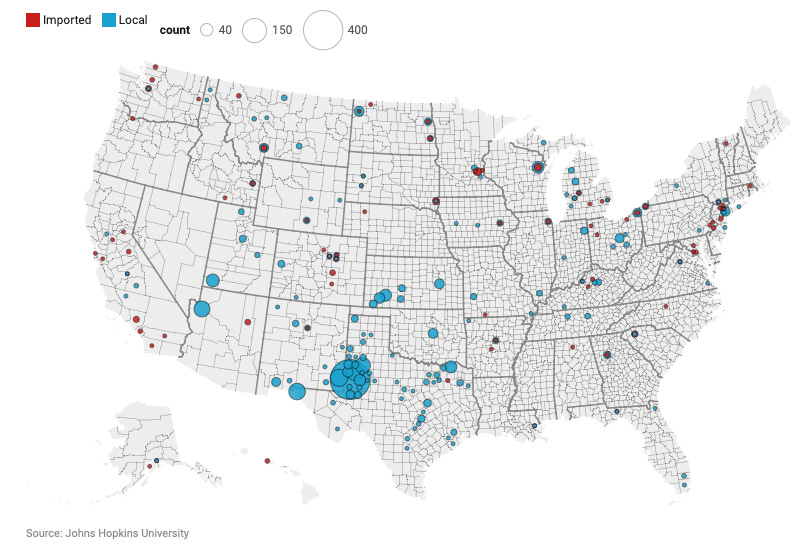
Distribution of reported U.S. cases:
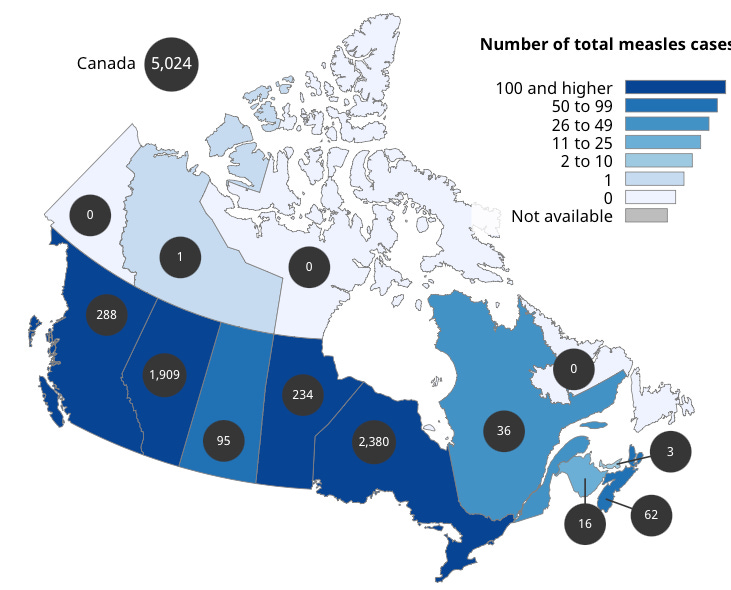
Canadian health authorities have reported 5,024 confirmed measles cases in 2025 in 10 jurisdictions (Alberta, British Columbia, Manitoba, New Brunswick, Northwest Territories, Nova Scotia, Ontario, Prince Edward Island, Quebec, Saskatchewan), with most cases related to an outbreak that began in New Brunswick in October 2024, with two deaths reported, both involving congenital measles in pre-term infants, one in Ontario & one in Alberta.
Canadian health authorities provide updated reports weekly on Mondays, here).
Mexico has reported 4,353 confirmed measles cases as of September 4 (up from 7 cases in 2024), with 14 deaths, with the state of Chihuahua reporting 3,778 confirmed and 5,286 suspected cases, and 13 deaths.
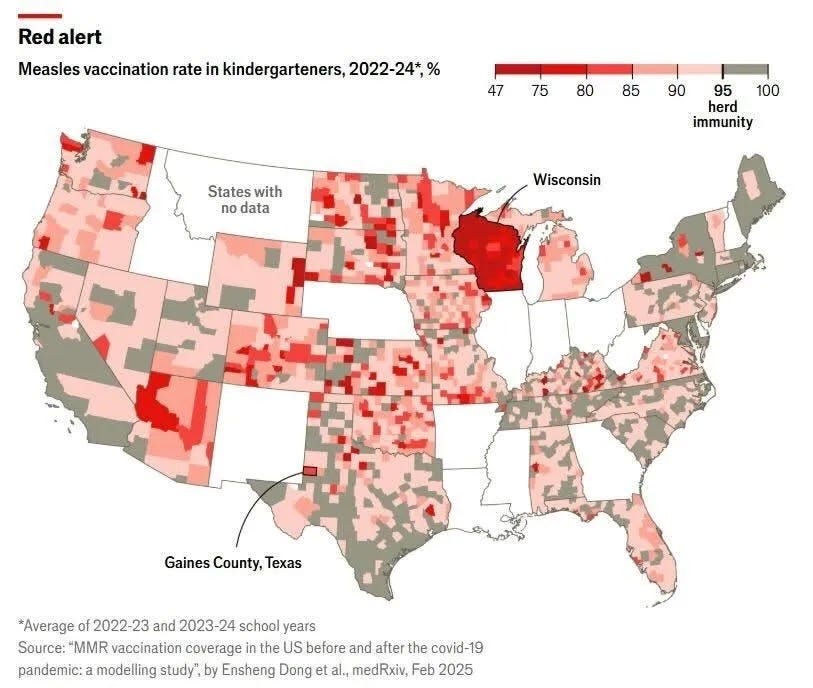
The outbreaks in Canada and the U.S. do not appear to be directly related, and appear to represent independent importations from regions of measles endemicity by residents returning from international travel (notably not by immigrants; missionary workers returning from regions of endemicity very commonly are the sources of importation), principally of the D8, D4, and B3 viral genotypes, all prominent in worldwide circulation (although we can identify several measles viral genotypes, these all belong to a single serotype, with all known genotypes covered by the vaccine). There appear to have been multiple introductions into Canada from residents returning from international travel, one involving a traveller returning to New Brunswick from SE Asia in October 2024, with subsequent spread involving a large Mennonite gathering in New Brunswick with attendees from multiple Canadian provinces. The index case of the Chihuahuan outbreak was a 9-year-old unvaccinated Mennonite child returning from a family trip to Gaines County, Texas, the epicenter of the West Texas outbreak; the source of the West Texas outbreak is unknown, but also involves principally the D8 genotype. Unfounded rumors of circulating vaccine strain virus are false; attenuated vaccine strain measles virus has not been seen to circulate in a community or to revert to wild-type pathogenicity. Mennonite communities, which are epicenters of the measles outbreaks in Canada, the U.S., & Mexico, typically have low rates of vaccination, well below the coverage necessary to interrupt endemic transmission, tho there is no specific religious objection to vaccination among the Mennonite or other Anabaptist groups; the school-level coverage in the Mennonite community of Gaines County, Texas is only 46%, compared to 81% for the state as a whole. Prevention of community spread appears to require immunity from natural infection or vaccination of at least 95% of the population.
From the CDC:
Only those regions depicted in blue below & in grey above have vaccination coverage sufficient to contain endemic spread; & within these, there may exist geographic & demographic pockets with inadequate coverage.
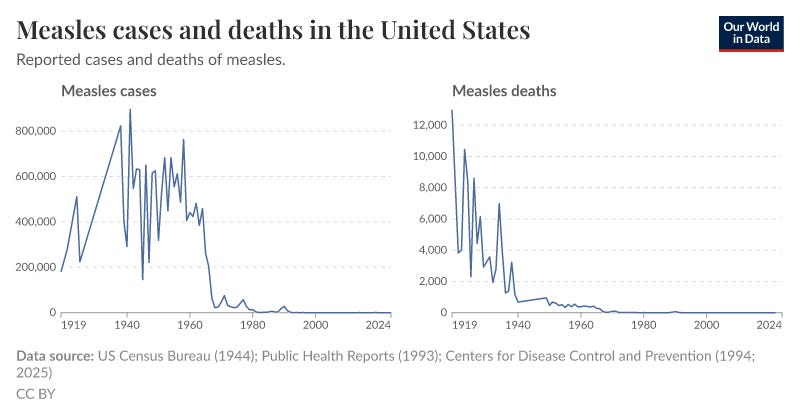
The numbers of measles cases, hospitalization, & deaths in these recent outbreaks are still relatively low in comparison to historical figures; in the 1950s, prior to introduction of measles vaccination, we saw an annual average of greater than 500,000 cases of measles (essentially every non-immune individual between the ages of 5-15 and some younger), 50,000 hospitalizations, and nearly 500 annual measles-related deaths (a 10% hospitalization rate & a case-fatality rate of 0.1%, figures that persist today) in the U.S. Add the cases of subacute sclerosing panencephalitis, invariably fatal, that may follow measles by 1 month to 27 years, at 2 per 10,000 cases, which at 500,000 cases annually would total 100 cases, morbidities involving vision & hearing loss, and the immunosuppression with loss of acquired immune memory following measles. These figures are often misrepresented in contemporary discussion, with some suggesting erroneously a grossly exaggerated death rate of 1 in 20, & others asserting that “60 years ago, we all got measles and no one died,” polarizing the discussion with inaccuracies in both extremes. This followed a dramatic decline in measles mortality & morbidity from the early 1900s, likely the result of improvements in Dickensian living conditions (but not in case numbers, which only declined following widespread adoption of vaccination in the mid-1960s, followed by a decline in the residual mortality of ~500 deaths annually).



Continues to be a very concerning "trend".
Thank you Dr. Will, for addressing and compiling this information!